Dr James Muecke Australian of the Year in 2020
There has been 7 articles in the Newcastle Herald during December 2021 and January 2022 relating to Dr James Muecke and Dr Peter Bruckner, a sport’s medical clinician, on how to prevent and cure diabetes with an animal-based diet that is high in fat and low in carbohydrates. Muecke and Bruckner both state that we should be eating more eggs, cheese, meat and dark chocolate to minimise diabetes, its associated blindness (diabetic retinopathy) and diabetic neuropathy.
One of these articles was an editorial “The pandemic should be all the impetus we need to properly address diabetes, the other silent assassin in our midst” urging people to address diabetes by adopting Dr Muecke and Dr Bruckner’s recommended diets.
Their recommendations are killing people.
Despite that these diets are not endorsed by the medical profession, both the Australian Medical Association and the Medical Journal of Australia have indicated that it is not within their scope to bring this to the attention of medical doctors or the Australian public.
The material below has been sent to the Newcastle Herald, The Australian newspaper, Sydney Morning Herald, my state and federal members of parliament, NSW and South Australia Health departments without obtaining any response.
WHO’s Draft Guidelines are Out of Date
On the 4th July 2019, the ABC published the following news item as its top news story.
World Health Organisation’s recommendations on saturated fat are out of date, expert team says. 1
It was based on an article published in THE BMJ the previous day, written by Arne Astrup and 17 colleagues, WHO draft guidelines on dietary saturated and trans fatty acids: Time for a new approach? 2
I made a complaint to the ABC regarding the accuracy of both the original BMJ article, and ABC’s article. I sent the journalist an 87 page A5 document, outlining many errors.
I received an email from the journalist on 24th September stating that, “I very much appreciate the time you’ve taken to get in touch and share your research with me, however, it’s not something I can act on at the moment.”
It is not responsible to leave the information published in ABC’s article to be uncorrected. The majority of readers will only see the statement,
The picture shows burger, chips, eggs, and baked beans.
The readers’ conclusion – eating bacon and eggs is no longer considered to be unsafe.
People do not need to read any further. They have already received the information that the wish to know.
The ABC’s editorial guidelines state, “Reasonable efforts must be made to ensure that material facts are accurate and presented in context.” and “factual content must not be presented in a way that will materially mislead the audience.”
At the end of Astrup’s article misleading evidence for including eggs, chocolate, cheese and meat is listed which matches the needs of their corporate sponsors.Dr James Muecke, the Australian of the Year in 2020, refers to this article to justify his high-fat, low-carbohydrate, high-animal based diet to minimise diabetes, its associated blindness (diabetic retinopathy) and diabetic neuropathy. Peripheral diabetic neuropathy is nerve damage of the limbs that is caused by diabetes. 50% of adults with type 2 diabetes have peripheral neuropathy. It can result in pain, numbness and an increase in sensitivity. Diabetes account for more than 80% of amputations. 3
Professor Robert Lustig, a paediatric endocrinologist at the University of California and author of Fat Chance: Beating the Odds against Sugar, Processed Food, Obesity, and Disease 4 who advocates that a high consumption of sugar is responsible for most of the diseases of affluence of modern civilisation. He states that,
My book – and video – documents how the food industry has manipulated the media and researchers to ensure that profits become before public health.
More detailed information can be obtained from the 17 page eBooklet Fat, Carbohydrate and Type 2 Diabetes.
Dr James Muecke is the Australian of the Year in 2020 which was awarded for his work as an eye-surgeon and his work in preventing blindness. He is trying to convince Australians to eat more meat, eggs and dairy. Australia is ranked number 2 in meat consumption, just behind United States but in front of Argentina, Uruguay, Brazil and New Zealand.
Muecke has declared that we need to “Declare war on type 2 diabetes and cut back on sugar” in order to reduce the incidence of blindness.
He believes that it is the introduction of sugary drinks and highly processed foods are the cause of diabetes – not a high-fat, high-protein diet as shown by numerous papers dating back to 1927. 5 6 7 8 9 10 11 12 13 14 15 16
According to the Australian Bureau of Statistics, the level of sugar consumption is decreasing. In 1995, the proportion of energy from free sugars was 12.5% compared with 10.9% in 2011-12 (10.9%), a decrease of 13%. This is still higher than the WHO recommendation of less than 10% of energy from free sugars. 17 Ideally, the consumption of free sugars should be close to zero.
Dr Muecke was interviewed by Keith Wheeler for a FarmOnline National article. Wheeler summed up his article with,
Muecke refers to a 2019 article in the Annals of Internal Medicine, Unprocessed Red Meat and Processed Meat Consumption: Dietary Guideline Recommendations From the Nutritional Recommendations (NutriRECS) Consortium to support his beliefs.
Walter Willett, the Harvard professor of epidemiology and nutrition, called the study
The publications produced by the NutriRECS organisation are concerned with proving that red meat consumption is healthy – or at least not detrimental.
Bradley Johnston is the director and co-founder of NutriRECS, and is an Associate Professor with the Departments of Nutrition & Statistics, Texas A&M University (formerly Agricultural and Mechanical College).
American College of Cardiology Review
The American College of Cardiology and the American Heart Association produced a 25 page review that examined the medical literature with the goal of developing “clinical practice guidelines for assessment of cardiovascular risk, lifestyle modifications to reduce cardiovascular risk, management of blood cholesterol in adults, and management of overweight and obesity in adults“. 20
This review examined three critical questions (CQs)
Critical Question 1 (CQ1)
Among adults, what is the effect of dietary patterns and/or macronutrient composition on CVD risk factors, when compared with no treatment or with other types of interventions?
Critical Question 2 (CQ2)
Among adults, what is the effect of dietary intake of sodium and potassium on CVD risk factors and outcomes, when compared with no treatment or with other types of interventions?
Critical Question 3 (CQ3)
Among adults, what is the effect of physical activity on BP and lipids when compared with no treatment or with other types of interventions?
In the FarmOnline article, Muecke states,
This is interesting as the review did not examine longevity or mortality. The review specifically states that,
Dr Muecke and Saturated Fat
Dr Muecke claims that 40 years of misguided ‘healthy eating’ advice have led to a dietary disaster in Australia and an explosion in rates of chronic disease including diabetes, now leading the cause of blindness in this country. 21
Australian Dietary Guidelines tell Australians to eat less saturated fat, “yet there is no evidence to suggest the natural saturated fat in our diet is linked to cardiovascular disease”, according to Muecke.
Muecke states that “Indeed, such fats are critical to our health, to our survival.”
Dr Muecke states there is “no evidence whatsoever” to link whole fat dairy, unprocessed red meat and eggs with heart attack, stroke and type 2 diabetes.
“Foods that have been demonised by our guidelines since their inception,” he said.
“This lack of evidence was well known in 2009 when the last review commenced, but this critical piece of evidence was seemingly ignored.”
“Instead of promoting healthy saturated fats the guidelines encouraged the eating of unhealthy polyunsaturated oils, and this in turn has led to the boom in the production and consumption of margarines and seed oils, industrially produced fats which have been linked to cardiovascular disease,” he said.
There is a lack of information in what is consumed in USA, Australia, New Zealand and Europe because of the cost of performing dietary surveys. The percentiles of macro nutrients (fat, protein, carbohydrates, saturated fats, trans-fats, as well as poly and mono saturated fats are not available. Japan is the exception.
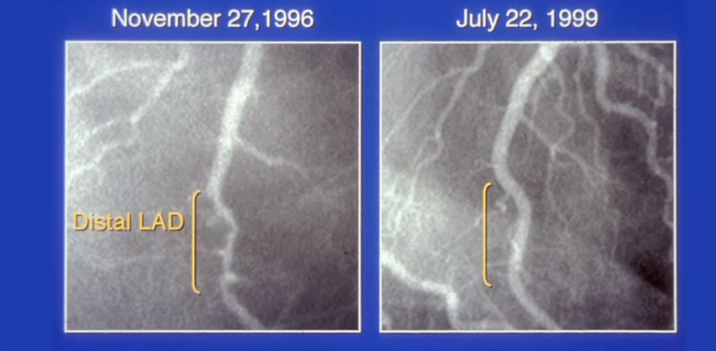
Below shows an example from Caldwell Esselstyn of the repair of a coronary artery. This result is not possible on Dr Muecke’s high-fat, high animal-based diet. 22 ~ 23
The average as well as the median (the middle value of the data) in the USA is approximately 34%. USA recommendations are 30% fat, 5%-10% poly-unsaturated fat and 15%-20% mono-unsaturated fat which is much higher than optimal.
A healthy whole-food, plant-based diet with no added oils is approximately 10% fat.
Dr Muecke cannot explain why the healthiest population on the planet are vegan Seventh-day Adventists of Loma Linda, California, who are even healthier than the Okinawans of southern Japan.
The average percentage of macronutrients consumed in the USA is shown below. 34% of the diet obtained from fats is NOT a low-fat diet.
| Protein | Carbohydrate | Fat | Saturated fat | Mono-unsaturated fat | Poly-unsaturated fat |
|---|---|---|---|---|---|
| 17% | 48% | 34% | 11% | 12% | 8% |
According to Eric Rimm, the famed Harvard epidemiologist, 24
Professor Walter Willet, the Harvard epidemiologist and Director of the Harvard Nurses’ Study states: 25
There has been three large Adventist cohort studies in the United States and Canada since the 1950s. 26
The diet of Seventh-day Adventists is significantly different from the general population.
- 4.2% are total vegetarian
- 31.6% lacto-ovo-vegetarian
- 11.4% include fish with their lacto-ovo-vegetarian diet
- 6.1% are semi-vegetarian (eat meat <1 time/week)
- 46.8% are non-vegetarian
The AHS-1 study showed 30-year-old Adventist males lives 7.3 years longer than the average 30-year-old white Californian male and with females living 4.4 years longer than the average Californian white female.
For vegetarians it is 9.5 years longer for men and 6.1 years longer for women.
The rate of breast and prostate cancer is 4 times greater in the US population than is experienced by the Adventists. Similarly, the rate of cardiovascular disease is 5 times greater in the general population.
These rates refer to all Seventh-day Adventists – not only those who avoid animal products.
Women’s Health Initiative
The Women’s Health Initiative was included in Johnston’s review and given a high grading as it is a randomised intervention trial. 27 28.
This study is frequently mentioned as a low-fat diet study that fails to improve health indicators.
The Dietary Modification trial of the Women’s Health Initiative evaluated the effect of a “low-fat” and high-fruit, vegetable-and-grain diet on the prevention of breast and colorectal cancers, and coronary heart disease in post-menopausal women. The participants followed either their usual eating pattern or a “low-fat” dietary pattern. 48,835 postmenopausal women in the United States participated in the trial with 40% assigned to the intervention group and the control group ws the remaining 60%.
The women self-reported their diets. According to the study, the intervention consisted of:
This was achieved by holding 18 group sessions in the first year and quarterly maintenance sessions afterwards for the intervention group. It could be disputed that this constitutes intensive behaviour modification, especially given the fact that behaviour did not change.
The widely-reported conclusion from this study informed readers that:
The effectiveness of a diet is much more that sum of the macronutrients. The participants failed to reach even the modest goals of the vital components of fruit, vegetables, whole-grains and dietary fibre. The average whole-grain, fruit and vegetable consumption was decreased.
One of the conclusions of this large study was,
Given that there was so little change in the diet of the intervention group over the six years then it is not surprising that the results did not show a reduction in the risk of heart disease and stroke.
There are also ethical issues with this kind of study. For any lifestyle change, participants and their families need to be committed to the concept. Randomly assigning participants to a particular group is not conducive to a positive outcome. Do we really need a random trial that lasts for a number of years, wait for the results to be analysed and published to find out that what we eat is really important?
The participants in the control group and intervention group were overweight and unhealthy at the start of the trial. (Control: average weight 76.8kg, BMI 29.1; Intervention: average weight 76.7kg, BMI 29.1)
Both groups were still overweight and unhealthy by the end of the trial. (Control: average weight 76.1 kg, BMI 29.2; Intervention: average weight 75.7kg, BMI 29.0)
Teicholz’s 2015 BMJ Article
On 23 September, 2015, another BMJ article was published by Nina Teicholz, The scientific report guiding the US dietary guidelines: Is it scientific? 29
It asks the question,
The author is wanting information on the benefits of saturated fats, animal products and low-carbohydrate diets to be included in the guidelines.
The next day, The BMJ issues this press release stating,
The press release failed to mention that nature of the BMJ investigation, the name of the expert report or the name of the committee that produced the report. The expert report is the Scientific Report of the 2015 Dietary Guidelines Advisory Committee. 30
At the end of the article in The BMJ, written by Teicholz, it clearly states:
I sent an email was sent to The BMJ and the following response on 29 June 2017 at 20:04.
The Laura and John Arnold Foundation provided the seed funding for The Nutritional Science Initiative organisation, NuSI, that was founded by Gary Taubes, and Peter Attia to promote low-carbohydrate nutritional science. 31
Nutrition and Randomised Clinical Trials
Whilst medical researchers love to quote that randomised clinical trials represent a “gold standard” of research, it is very difficult to perform randomised clinical trials with nutrition.
With drug trials where the only variable is the drug is being tested it is easy to design a study where neither the participants or the researchers are aware of which individual received the treatment.
A number of researchers studied the relationship of saturated fat to serum cholesterol during the 1950s including Ancel Keys replaced saturated fats in the diet with polyunsaturated fats. All other components of the diet remained the same and the total fat content of the diet did not change. 32 33
For the duration of the studies the participants consumed a liquid concoction with different types of lipids. When the unsaturated fats, such as corn or safflower oil, were replaced by the saturated fats of butter, lard, or coconut oil, the serum cholesterol rose. The serum cholesterol fell when the polyunsaturated fats were reintroduced.
The experiments were repeated, and whilst there was variability with the amount of change for different individuals, the results were consistent for each individual. The changes occurred rapidly within one or two weeks.
Both the American College of Cardiology and the Johnston review give higher credence to randomised studies irrespective of their quality. Observational studies are given less credence or ignored.
All studies are comparing the results from two or more cohorts. The careful choice of the control group can completely skew results.
Low-carbohydrate or ketogenic dietary trials almost invariably are comparing overweight or obese participants, often on an energy-restricted, improbable diets before announcing that weight loss or diabetic control has been improved on their low-carbohydrate diets when compared with their version of a “low-fat” diet. The comparison “low-fat” diet is invariably an unhealthy diet with a fat intake of about 30%. This is NOT a low-fat diet. The average American, Canadian and US diets have a fat intake of 33%.34 35 36 37 38 39
Conflicting Evidence
There are thousands of studies that refute the basic premises of Johnston’s and Astrup’s papers. Three studies are examined below.
Causes of Type 2 Diabetes
If you type “intramyocellular lipids diabetes” into a Google Scholar search, you will receive hundreds of search results. This refers to fats inside muscle cells. The type of fat is irrelevant. 12 13 14 15 16
Normally, insulin attaches to protein receptors on the cell’s surface and signals the cell membrane to allow glucose to enter. If there is an accumulation of fat in the cell, it interferes with insulin’s signalling process and glucose cannot enter the cell. Fat can accumulate inside muscle cells even in slim people. The real cause of type 2 diabetes is not an excess of sugar or carbohydrates. It is an accumulation of fat inside the cells that interferes with the muscle cells’ ability to respond to insulin. The muscle cells are unable to access glucose, which is required for energy production.
As the papers above indicate, these changes can happen overnight.
Sweeney Studies from 1927
The result of Type 2 diabetes is that the body does not process sugar effectively, which results in high levels of glucose in the blood. High levels of glucose over an extended period of time places you at risk for many serious health problems. The usual medical advice is to prescribe a diet with very little sugar and limit starch in the diet since glucose is formed as a result of starch being digested. This does seem to be the logical solution to having too much glucose in the blood.
It has been known since at least 1927 that high fat diets increase insulin resistance. Healthy, young medical students were divided into four dietary groups: 5 6
- high-carbohydrate diet consisting of sugar, candy, syrup, baked potatoes, bananas, and oatmeal, rice, and white bread
- high-fat diet consisting of olive oil, butter, mayonnaise, egg-yolks and cream
- high-protein diet consisting of lean meat, lean fish, and egg-whites
- the fourth group was placed on a fasting regime

The students were fed their diets for two days and a glucose tolerance test (GTT) was performed on the morning of the third day. The students who consumed the high-carbohydrate showed an increase in tolerance for dextrose; those on the high-protein diet showed a mild inability to remove sugar from the blood; those on the high-fat and starvation diets showed a significant decrease in their tolerance for sugar.
Seventh-day Adventist Studies
A strong commitment to health has been a part of Adventist’s tradition since its founding in the 1840s. There has been three large Adventist cohort studies in the United States and Canada. These studies have generated hundreds of papers, which give a valuable insight to diet and the implication for our health.
As the diet becomes more vegetarian, so the risk of diabetes is reduced. Note the comparison is with non-vegetarian Seventh-day Adventists who are much healthier than the average American. Also, adjustments are made for data that is not necessarily independent. 40
| Category | % | BMI | Type 2 diabetes Odds ratio (*) |
|---|---|---|---|
| Vegan No red meat, fish, poultry, dairy, eggs | 4.2 | 23.6 | 0.32 |
| Lacto-ovo vegetarians Vegan with eggs and milk | 31.6 | 25.7 | 0.43 |
| Pesco-vegetarians Vegan with fish, milk and eggs | 11.4 | 26.3 | 0.56 |
| Semi-vegetarians Red meat, poultry less than once a week plus fish, milk, and eggs | 6.1 | 27.3 | 0.69 |
| Non-vegetarians Red meat, poultry more than once a week plus fish, milk, and eggs | 46.9 | 28.8 | 1 |
(*) After adjustment for age, sex, ethnicity, education, income, physical activity, television watching, sleep habits, alcohol use and BMI.
The reference group of non-vegetarians is much healthier than the control groups from the Women’s Health Initiative and the ketogenic diet studies. Alcohol use, smoking and meat consumption is much lower than in Seventh-day Adventist populations than the standard American population.
The adjustments for BMI, physical activity, television watching are not independent variables so the results can be skewed unfavourably away from the vegetarian diets.
Much publicity is given to the longevity of the people of Japan and Okinawa (an archipelago that stretches from southern Japan to Taiwan). However, it is vegetarian Californian Seventh-day Adventists that have the longest lifespan and the highest levels of health on the planet.
Vegetarian Californian Adventists have a higher lifer expectancy at the age of 30 years than other white Californians by 9.5 years in men and 6.1 years in women, giving them the highest life expectancy of any formally described population. 26
Note that Californians are much healthier than the average American being in the top five states for longevity with an average life expectancy of 5-6 years greater than the Mississippi states.
Taiwanese Buddhist Study
A Taiwanese Buddhist study with 4,384 participants compared type 2 diabetes outcomes for lacto-ovo-vegetarians compared with those who consumed meat. The meat-eating group ate only a very small amount of meat. 41
- intake for females: 50% consumed less than 10 g/day; 25% consumed less than 2 g/day.
- Meat intake for males: 50% consumed less than 20 g/day; 25% consumed less than 7 g/day.
- Fish and meat intake for females: 50% consumed less than 17 g/day; 25% consumed less than 3 g/day.
- Fish and meat intake for males: 50% consumed less than 37 g/day; 25% consumed less than 11 g/day.
There were insufficient numbers to divide the vegetarians into subgroups (pesco, lacto-ovo, vegan). There were 69 vegans (no animal products) and there were no cases of diabetes within this group.
One Big Mac, with 2 meat patties, contains 90 g of meat—so the participants were consuming only a very small amount of meat. Three garden peas weigh a gram.
That minute amount of meat increased the risk of diabetes 4 times for females and 2 times for males.
| Category | Pre-menopausal women | Menopausal women | Men | |||
|---|---|---|---|---|---|---|
| Diet type | Vegetarian | Omnivore | Vegetarian | Omnivore | Vegetarian | Omnivore |
| Diabetes % | 0.6 | 2.3 | 2.8 | 10 | 4.3 | 8.1 |
| Impaired Fasting Glucose % | 5.8 | 9.0 | 14 | 18 | 12 | 17 |
The control group is much healthier than the control groups from the Women’s Health Initiative and the ketogenic diet studies.
Egg Consumption and Diabetes in Jiangsu Province
To assess the impact of egg consumption on type 2 diabetes in China, a survey was performed among 2849 adults in Jiangsu Province, China. Jiangsu is a coastal Chinese province north of Shanghai. 42
Dietary information was obtained by a validated food frequency questionnaire and 3 day weighed food records. Note that this survey did not rely on dietary recall.
Egg consumption was significantly and positively associated with diabetes risk. Below is the risk of diabetes according to egg consumption.
| Egg Consumption | Women Odds Ratio | Men Odds Ratio |
|---|---|---|
| Less than 2 eggs per week | 1.00 | 1.00 |
| 2-6 eggs per week | 1.67 | 2.03 |
| 1 egg per day or greater | 3.22 | 2.44 |
Plasma triglyceride and total cholesterol levels were also significantly higher in women who consumed more than 2 eggs/week than those who consumed eggs less often.
The conclusion of this paper is,
The Allure of Low-Carbohydrate Diets
There are many doctors (including my doctor) and health professionals who believe that a low-carbohydrate diet, one rich in fat and protein diet is beneficial. These diets are rich in animal-sourced products.
In 2018, 36% of Australians aged 18 and over are overweight (BMI of 25 to up to 30) and 31% of the population are obese (BMI 30 or more). 43
34% of adult Australians have hypertension (greater than 140/90 or taking medication). 44
According to the Framingham Risk Assessment calculator, a systolic value of less than 120 mmHg is ideal.
5.3% of Australian adults aged 18 and over had type 2 diabetes in 2017–18. Diabetes is the fastest growing chronic condition in Australia, increasing at a faster rate than other chronic diseases such as heart disease and cancer. 45
Between 25% and 35% of Australians diabetics report some form of diabetic retinopathy. 46
Something is seriously wrong and the situation is becoming worse.
There are a multitude of websites advocating low-carbohydrate and ketogenic diets – far more than those advocating whole-food, plant-base diets. People enjoy their high-fat, animal-based diets and do not require much encouragement to increase their consumption.
If carbohydrates are limited in the diet that means an increase in fats, proteins and animal-based foods. Those offering low-carbohydrate dietary plans usually offer (expensive) supplements to make up for the deficiencies of their diets.
Dr Muecke is passionate about his crusade to prevent diabetes, its associated blindness (diabetic retinopathy), diabetic neuropathy and amputations. Unfortunately, the solution is based on popular myths and as a result is contributing to society’s ill-health. No-one has the courage to gently point our that the “facts” Dr Muecke is presenting to the Australian public does not hold up to scrutiny.
Eliminating sugar from the diet is a simplistic message. Foods are much more than the sum of fats, protein and carbohydrates. A whole-food, plant-based diets automatically removes added sugars and oils. This results in a diet high in fibre, complex carbohydrates, micronutrients, antioxidants, vitamins, minerals and thousands of phytonutrients such carotenoids and flavonoids. Individual components do not work in isolation but work synergistically.
Last updated on Friday 16 August 2024 at 16:13 by administrators
Footnotes
- Taylor, T. (2019) World Health Organisation’s recommendations on saturated fat are out of date, expert team says – Health – ABC News [online]. Available from: https://www.abc.net.au/news/health/2019-07-04/who-saturated-fat-recommendations-out-of-date-expert-team-says/11274136 (Accessed 5 July 2019).
- Astrup, A. et al. (2019) WHO draft guidelines on dietary saturated and trans fatty acids: time for a new approach? BMJ. 366 (366), l4137.
- Hicks, C. W. & Selvin, E. (2019) Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Current Diabetes Reports. 19 (10), 86
- Lustig, R. (2013) Fat Chance: Beating the Odds Against Sugar, Processed Food, Obesity, and Disease. New York: Penguin Group.
- Sweeney, J. S. (1927). Dietary Factors that Influence the Dextrose Tolerance Test. Archives of Internal Medicine, 40(6), 818–830.
- Sweeney, J. S. (1928). A comparison of the effects of general diets and of standardized diets on tolerance for dextrose. Archives of Internal Medicine, 42(6), 872–876.
- Gale, E. A. (2013) Commentary: The hedgehog and the fox: Sir Harold Himsworth (1905–93). International Journal of Epidemiology. 12 (6), 1602–1607
- Black, D. & Gray, J. (1995) Sir Harold Percival Himsworth, K. C. B., 19 May 1905 – 1 November 1993.
- Himsworth, H. P. (1935) Diet and the incidence of diabetes mellitus. Clinical Science. 2117–148.
- Himsworth, H. P. (1934) Dietetic factors influencing the glucose tolerance and the activity of insulin. The Journal of Physiology. 29–48.
- Himsworth, H. & Marshall, E. (1935) The diet of diabetics prior to the onset of the disease. Clinical Science. 295–115.
- Bachmann, O. P., Dahl, D. B., Brechtel, K., Haap, M., Maier, T., Loviscach, M., … Jacob, S. (2001). Effects of Intravenous and Dietary Lipid Challenge on Intramyocellular Lipid Content and the Relation With Insulin Sensitivity in Humans. Diabetes, 50(13), 2579–2584.
- Jacob, S., Machann, J., Rett, K., Brechtel, K., Volk, A., Renn, W., … Häring, H.-U. (1999). Association of Increased Intramyocellular Lipid Content With Insulin Resistance in Lean Nondiabetic Offspring of Type 2 Diabetic Subjects. Diabetes, 48(21), 1113–1119.
- Krssak, M., Falk Petersen, K., Dresner, A., DiPietro, L., Vogel, S. M., Rothman, D. L., … Roden, M. (1999). Intramyocellular lipid concentrations are correlated with insulin sensitivity in humans: A 1H NMR spectroscopy study. Diabetologia, 42(1), 113–116.
- Roden, M., Krssak, M., Stingl, H., Gruber, S., Hofer, A., Furnsinn, C., … Waldhausl, W. (1999). Rapid impairment of skeletal muscle glucose transport/phosphorylation by free fatty acids in humans. Diabetes, 48(2), 358–364.
- Roden, M., Price, T. B., Perseghin, G., Petersen, K. F., Rothman, D. L., Cline, G. W., & Shulman, G. I. (1996). Mechanism of free fatty acid-induced insulin resistance in humans. Journal of Clinical Investigation, 97(12), 2859–2865.
- Australian Bureau of Statistics (2016) Australian Health Survey – Consumption of Added Sugars Australia 2011-12. p15
- Oreskes, N. (2020) So Is It Okay to Eat More Red and Processed Meat? Scientific American. 322 (2), 70.
- Mole, B. (2020) Researcher promoting red meat, sugar failed to disclose industry ties—again | Ars Technica
- Eckel, R. H. et al. (2014) 2013 AHA/ACC Guideline on Lifestyle Management to Reduce Cardiovascular Risk. Journal of the American College of Cardiology. 63 (25), 2960–2984.
- Nelson, J. (2021) Australian of the Year ophthalmologist blasts flawed Dietary Guidelines. Available from: https://www.beefcentral.com/news/australian-of-the-year-ophthalmologist-blasts-flawed-dietary-guidelines/.
- Left Anterior Descending Artery
- Esselstyn, C. B. (2007) Prevent and Reverse Heart Disease. New York: Penguin Group
- Fox, M. (2002) Trans-fat increase cholesterol levels [online]. Available from: http://jawawa.id/index.php/newsitem/trans-fat-increase-cholesterol-levels-1447893297 (Accessed 29 March 2017).
- Kolata, G. (1990) Animal Fat is Tied to Colon Cancer – New York Times [online]. Available from: http://www.nytimes.com/1990/12/13/us/animal-fat-is-tied-to-colon-cancer.html (Accessed 28 January 2017).
- Fraser, G. E., & Shavlik, D. J. (2001). Ten Years of Life—Is It a Matter of Choice? Archives of Internal Medicine, 161(13), 1645–1652.
- Howard, B. V. et al. (2006) Low-Fat Dietary Pattern and Risk of Cardiovascular Disease: The Women’s Health Initiative Randomized Controlled Dietary Modification Trial. Journal of the American Medical Association. 295 (6), 655.
- Howard, B. V. et al. (2006) Low-Fat Dietary Pattern and Weight Change Over 7 Years: The Women’s Health Initiative Dietary Modification Trial. Journal of American Medical Association. 295 (1), 39
- Teicholz, N. (2015). The scientific report guiding the US dietary guidelines: Is it scientific? BMJ, 351, h4962.
- Dietary Guidelines Advisory Committee. (2015). Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Retrieved from https://health.gov/dietaryguidelines/2015-scientific-report/
- Taubes, G. (2012, September 12). The Launch of The Nutrition Science Initiative. Retrieved June 26, 2017, from http://garytaubes.com/the-launch-of-the-nutrition-science-initiative/
- Keys, A. et al. (1959) Serum Cholesterol in Man: Diet Fat and Intrinsic Responsiveness. Circulation. 19 (2), 201–214.
- Keys, A. et al. (1960) Diet-type (fats constant) and blood lipids in man. The Journal of Nutrition. 70 (2), 257–266.
- Westman, E. C. et al. (2008) The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutrition & Metabolism. 5 (1), 36.
- Volek, J. S. et al. (2009) Carbohydrate Restriction has a More Favorable Impact on the Metabolic Syndrome than a Low Fat Diet. Lipids. 44 (4), 297–309.
- Yancy, W. S. et al. (2004) A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Annals of Internal Medicine. 140 (10), 769–777.
- Tay, J. et al. (2015) Comparison of low- and high-carbohydrate diets for type 2 diabetes management: a randomized trial. American Journal of Clinical Nutrition. 102 (4), 780–790.
- Tay, J. et al. (2014) A Very Low-Carbohydrate, Low–Saturated Fat Diet for Type 2 Diabetes Management: A Randomized Trial. Diabetes Care. 37 (11), 2909–2918.
- Brinkworth, G. D. et al. (2009) Long-term effects of a very-low-carbohydrate weight loss diet compared with an isocaloric low-fat diet after 12 mo. American Journal of Clinical Nutrition. 90 (1), 23–32.
- Tonstad, S., Butler, T., Yan, R., & Fraser, G. E. (2009). Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care, 32(5), 791–796.
- Chiu, T. H. T., Huang, H.-Y., Chiu, Y.-F., Pan, W.-H., Kao, H.-Y., Chiu, J. P. C., Lin, M.-N., & Lin, C.-L. (2014). Taiwanese Vegetarians and Omnivores: Dietary Composition, Prevalence of Diabetes and IFG. PLoS ONE, 9(2), e88547.
- Shi, Z., Yuan, B., Zhang, C., Zhou, M., & Holmboe-Ottesen, G. (2011). Egg consumption and the risk of diabetes in adults, Jiangsu, China. Nutrition, 27(2), 194–198.
- Australian Bureau of Statistics. (2018, December 12). Overweight and obesity, 2017-18 financial year | Australian Bureau of Statistics. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/overweight-and-obesity/latest-release
- Australian Institute of Health and Welfare. (2019, July 19). High blood pressure, High blood pressure—Australian Institute of Health and Welfare. https://www.aihw.gov.au/reports/risk-factors/high-blood-pressure/contents/high-blood-pressure
- Australian Institute of Health and Welfare. (2020, July 15). Diabetes, Type 2 diabetes—Australian Institute of Health and Welfare. https://www.aihw.gov.au/reports/diabetes/diabetes-snapshot/contents/how-many-australians-have-diabetes/type-2-diabetes
- Diabetes Australia. (2020). Diabetes in Australia – Diabetes Australia. https://www.diabetesaustralia.com.au/about-diabetes/diabetes-in-australia/



One Reply to “Dr James Muecke Australian of the Year in 2020”