The Keto diet slays the opposition? – not true
An article titled, How the Keto diet – even without exercise – slays the opposition, by Derek Beres was published on Think Big website on 11th December 2017. 1
Derek is a yoga and fitness instructor based in Los Angeles and author of the book Whole Motion: Training Your Brain and Body for Optimal Health. He advocates a diet based on the KETO Food Pyramid.
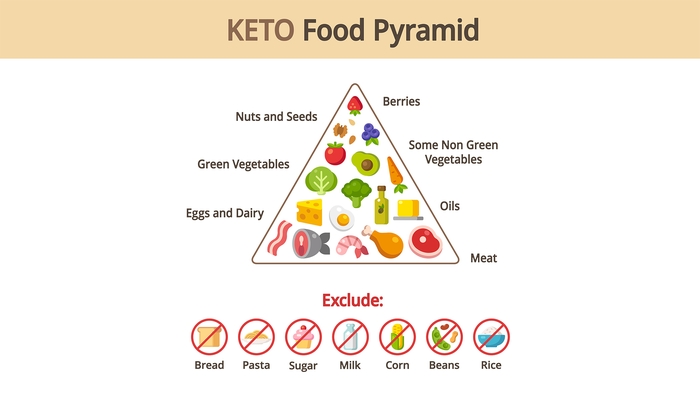
Derek advocates shunning rice (which is eaten by healthy Asians), corn & beans (eaten by healthy Hispanics and people of Central America) and bread & pasta (eaten by healthy Mediterranean communities) in favour of meat – eaten by unhealthy Americans, Europeans and Inuits.
He quotes a study by Gibas and Gibas to support his claim. The Gibas article contends that ketosis is a useful and valid tool to control metabolic syndrome, diabetes and obesity. 2
Metabolic syndrome has not been defined in this paper.
The Adult Treatment Panel (ATP) III, definition that it consists of at least 3 of the following 5 conditions. 3
- waist circumference greater than 102 cm (40 in) in men and 88 cm (35 in) in women
- serum triglycerides concentration of at least 150 mg/dL (1.7 mmol/L)
- serum high-density lipoprotein cholesterol concentration of less than 40 mg/dL in men and 50 mg/dL in women (1.0 mmol/L men and 1.3 mmol/L women)
- blood pressure of at least 130/85 mmHg
- serum glucose concentration of at least 110 mg/dL (6.1 mmol /L)
The Gibas study examined 30 adults assessed by their doctor as having metabolic syndrome. All participants were overweight with a BMI of 25 or greater. 10 participants were randomly assigned to a ketogenic diet, 10 to a Standard American Diet and 10 to a Standard American Diet with exercise.
The references for this paper include a number of authors (J. Volek, R. Feiman, E. Westman) who have received funding from the Robert C. Atkins Foundation which supports research into low-carbohydrate nutrition.
The participants may have been randomly assigned to one of the three groups. However, the baseline measurements for weight were significantly different for the three groups which grossly distorts the results. For example, average weight for the ketogenic diet group was 240 pounds (109 kg) whilst the SAD (without exercise) was 190 pounds (86 kg) and SAD (with exercise) was 175 pounds (79 kg). Values are calculated from the graph as the original data is not provided.
The ketogenic diet consumed by the participants contained less than 30 g/day of carbohydrate. No other details of the diet were described. The alternative [the Ketogenic] diet has not been described. The adequacy of a diet cannot be defined in terms of the macronutrient content – that is the proportion of energy obtained from carbohydrate, fat and protein.
A multitude of other factors determine the viability of a diet including the total amount of energy, amount of fibre, antioxidants and the source of fat and protein. It is simplistic to measure the proportion of carbohydrates, fats and proteins to determine the quality of a diet.
The trial only lasted for ten weeks which is insufficient time to adequately assess long-term health outcomes and the criteria recorded to measure the health status of the participants are very selective.
Despite cholesterol being part of the definition of metabolic syndrome, this was not measured.
High-fat and ketogenic diets: 4 5 6
- Raise total cholesterol, LDL cholesterol, lipoprotein(a), triglycerides
- Homocysteine
- Fibrinogen and C-reactive protein (inflammation markers)
- Raise uric acid
- Raise IGF-1 which is associated with increased breast and prostate cancers
- Raise ketones (acetone, acetoacetate and β-hydroxybutyrate)
- Reduce coronary blood flow
- Reduce blood pH (blood becomes more acidic)
- Raise blood presssure
- Lower body temperature which reduces energy requirements
- Increase cortisol which is associated with stress
Seventh-day Adventist’s Studies
Seventh-day Adventist’s Studies (and many others) have shown that as the diet becomes more plant-based, the incidence of many ailments including obesity and diabetes decreases. 7
| Category | % | BMI | Type 2 diabetes Odds ratio (*) |
|---|---|---|---|
| Vegan No red meat, fish, poultry, dairy, eggs | 4.2 | 23.6 | 0.32 |
| Lacto-ovo vegetarians Vegan with eggs and milk | 31.6 | 25.7 | 0.43 |
| Pesco-vegetarians Vegan with fish, milk and eggs | 11.4 | 26.3 | 0.56 |
| Semi-vegetarians Red meat, poultry less than once a week plus fish, milk, and eggs | 6.1 | 27.3 | 0.69 |
| Non-vegetarians Red meat, poultry more than once a week plus fish, milk, and eggs | 46.9 | 28.8 | 1 |
(*) After adjustment for age, sex, ethnicity, education, income, physical activity, television watching, sleep habits and alcohol use.
Much publicity is given to the longevity of the people of Japan and Okinawa (an archipelago that stretches from southern Japan to Taiwan). However, the healthiest population on the planet is the vegan Californian Seventh-day Adventists. 8
Diabetes and Plant-based Diets
McDougall showed significant improvement in diabetic and cardiovascular markers after seven days on a low-fat, plant-based diet. Carbohydrate intake was approximately 80% of total energy with fat representing 10% or less. 9
The diet consisted of no animal-derived products or isolated vegetable oils. Meals included wheat flour products, corn, rice, oats, barley, quinoa, potatoes, sweet potatoes, beans, peas, lentil, fresh fruits and non-starchy green, orange, and yellow vegetables. The macro nutrient profile was approximately 7% fat, 12% protein, and 81% carbohydrate by energy consumption. After seven days, there was a substantial reduction to relevant bio-markers. The reduction occurred even though 86% of patients on blood pressure medications and 90% of patients on diabetes medications reduced their dosage or discontinued the medication.
Examine the extent of the changes that were made on the elevated markers after only 7 days on a low-fat, high-carbohydrate, whole-food, plant-based diet.
| Criteria | Units | Baseline Median | Day 7 Median | Δ | Δ % |
|---|---|---|---|---|---|
| Weight - Men | kg | 93.2 | 92.5 | -1.5 | -1 |
| Weight - Women | kg | 79.2 | 78.0 | -1.4 | -2 |
| Cholesterol | |||||
| • 150–179 at baseline | mg/dL | 165 | 146 | -20 | -12 |
| • 180–209 at baseline | mg/dL | 193 | 169 | -25 | -12 |
| • 210–239 at baseline | mg/dL | 221 | 188 | -34 | -15 |
| • ≥ 240 at baseline | mg/dL | 261 | 222 | -39 | -15 |
| Systolic blood pressure | |||||
| • Elevated (≥140) at baseline | mmHg | 150 | 136 | -18 | -9 |
| Triglycerides | |||||
| • Borderline high (150–199) | mg/dL | 169 | 157.5 | -11.5 | -7 |
| • High (200–499) | mg/dL | 247 | 216 | -46 | -13 |
| • Very high (≥500) | mg/dL | 569 | 360 | -294 | -37 |
| Glucose | |||||
| • < 100 | mg/dL | 88 | 86 | -1 | -2 |
| • 100 to 126 | mg/dL | 107 | 99 | -8 | -7 |
| • > 126 | mg/dL | 156 | 149 | -17 | -4 |
| Blood Urea Nitrogen | |||||
| • < 10 | mg/dL | 8 | 7 | -1 | -13 |
| • 10 to 20 | mg/dL | 13 | 9 | -4 | -31 |
| • > 20 | mg/dL | 23 | 14 | -10 | -39 |
| Creatinine | |||||
| • > 1.4 | mg/dL | 1.6 | 1.5 | 0.1 | -6 |
Barnard compared a low-fat, plant-based diet to an American Diabetes Association diet. The plant-based diet out performed that ADA diet and showed a significant improvement in all markers measured over the 22 weeks of the trial. 10
David Jenkins, the Toronto-based researcher who created the glycaemic index, and Neal Barnard are amongst the co-authors of a trial studying the impact of vegan diets on the management of type 2 diabetes.
Results were evaluated at 22 weeks and 74 weeks. The results below are from 22 weeks because these results distinguish between those participants that did not reduce their medication so it does not confound the results.
Nine vegan (completion rate 82%) and seven (completion rate 86%) from the ADA diet group did not complete the 74 week program, which is much higher than the completions rates for studies comparing high-fat, low-carbohydrate diets with “low-fat” diets. Note that 16 of the 49 vegan-group participants did not adhere strictly to their diet. Their cholesterol intake was reduced from an average of 291 mg/day to 24 mg/day. The ADA group reduced their intake from an average 317 mg/day to 189 mg/day. A vegan diet contains no cholesterol.
The changes for those who did not change their medications are more relevant as it removes the confounding influences of additional modifications to behaviour.
| Criteria | Vegan | ADA | ||||||
|---|---|---|---|---|---|---|---|---|
| Start | End | Change | % | Start | End | Change | % | |
| Cholesterol medications reduced | - | - | - | -10% | - | - | - | -9% |
| Diabetic medications reduced | - | - | - | -51% | - | - | - | -34% |
| Weight (kg) | 33.9 | 31.8 | -2.1 | -6% | 35.9 | 34.3 | -1.5 | -4% |
| BMI (kg / (m • m)) | 33.9 | 31.8 | -2.1 | -6% | 35.9 | 34.3 | -1.5 | -4% |
| HbA1C | 8.00 | 7.10 | -1.00 | -13% | 7.90 | 7.40 | -0.60 | -8% |
| HbA1C (Exc those who reduced medication) | 8.07 | 6.84 | -1.23 | -15% | 7.88 | 7.50 | -0.38 | -5% |
| Total cholesterol (mmol/L) | 4.84 | 4.13 | -0.72 | 15% | 5.15 | 4.52 | -0.63 | -12% |
| Total cholesterol (mmol/L) (Exc those who reduced medication) | 4.93 | 4.06 | -0.87 | -18% | 5.05 | 4.56 | -0.49 | -10% |
| LDL cholesterol (mmol/L) | 2.70 | 2.28 | -0.42 | -16% | 3.07 | 2.67 | -0.40 | -13% |
| LDL cholesterol (mmol/L) (Exc those who reduced medication) | 2.78 | 2.19 | -0.59 | -21% | 2.99 | 2.71 | -0.28 | -9% |
| Urinary albumin (mg/24 h) | 33.0 | 14.6 | -18.4 | -56% | 55.0 | 43.7 | -11.3 | -21% |
The Cause of Diabetes
Sweeney showed in 1927 that high-fat diets increase insulin resistance. 11 12
Students were fed their diets four highly improbable diets for two days: a high-fat diet, high-carbohydrate diet, high-protein diet and a fasting diet. A glucose tolerance test was performed on the morning of the third day.
After only two days on their experimental diets, the only group showing a normal, healthy response to the glucose tolerance test was the high-carbohydrate group. Both the high-fat and fasting diet showed – after only two days – a significant increase in insulin resistance.
The relationship between an increase in fats in muscle cells and insulin resistance has been documented since the late 1990s. 13 14
Normally, insulin attaches to protein receptors on the cell’s surface and signals the cell membrane to allow glucose to enter. If there is an accumulation of fat in the cell, it interferes with insulin’s signalling process and glucose cannot enter the cell. Fat can accumulate inside muscle cells even in slim people. The real cause of type 2 diabetes is not an excess of sugar or carbohydrates. It is an accumulation of fat inside the cells that interferes with the muscle cells ability to respond to insulin. The muscle cells are unable to access glucose, which is required for energy production.
Type 2 diabetes does result in an increase in glucose in the blood and urine but this does not mean that type 2 diabetes is caused by a consumption of sugars or carbohydrates.
Derek is the author of Whole Motion: Training Your Brain and Body For Optimal Health. He states that he is working on a new book about spiritual consumerism.
Slaughtering 8 billion animals annually in the US for “food” is not an example of spiritual consumerism.
Consuming animal protein production that requires more than eight times as much fossil-fuel energy than the production of plant protein, is not an example of spiritual consumerism. 15
Consuming beef that requires 100,000 litres of water for every kilogram of food compared with soy production (2,000 litres for kilogram), rice (1,900 litres), wheat (900 litres) and potatoes (500 litres) is not an example of spiritual consumerism. 15
Producing beef consumes:
- 50 times more water than soy
- 52 times more water than rice
- 110 times more water than wheat
- 200 times more water than potatoes
Other posts relating to low-carbohydrate diets and ketogenic diets.
Last updated on Tuesday 21 March 2023 at 01:31 by administrators
Footnotes
- Beres, D. (2017) How the Keto diet—even without exercise—slays the opposition | Big Think [online]. Available from: bigthink.com/21st-century-spirituality/how-the-keto-diet-with-no-exercise-outperforms-the-standard-american-diet-with-exercise (Accessed 1 March 2018).
- Gibas, M. K. & Gibas, K. J. (2017) Induced and controlled dietary ketosis as a regulator of obesity and metabolic syndrome pathologies. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 11S385–S390.
- Ford, E. S. et al. (2002) Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. Journal of American Medical Association. 287 (3), 356–359.
- Fleming, R. M. (2002) The Effect of High-, Moderate-, and Low-Fat Diets on Weight Loss and Cardiovascular Disease Risk Factors. Preventive Cardiology. 5 (3), 110–118.
- Fleming, R. M. & Boyd, L. B. (2000) The effect of high-protein diets on coronary blood flow. Angiology. 51 (10), 817–826.
- Ballaban-Gil, K. et al. (1998) Complications of the Ketogenic Diet. Epilepsia. 39 (7), 744–748.
- Tonstad, S. et al. (2009) Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care. 32 (5), 791–796.
- Fraser, G. E. & Shavlik, D. J. (2001) Ten Years of Life – Is It a Matter of Choice? Archives of Internal Medicine. 161 (13), 1645–1652.
- McDougall, J. et al. (2014) Effects of 7 days on an ad libitum low-fat vegan diet: the McDougall Program cohort. Nutrition Journal. 13 (99), 1–7.
- Barnard, N. D. et al. (2006) A Low-Fat Vegan Diet Improves Glycemic Control and Cardiovascular Risk Factors in a Randomized Clinical Trial in Individuals With Type 2 Diabetes. Diabetes Care. 29 (8), 1777–1783.
- Sweeney, J. S. (1927) Dietary Factors that Influence the Dextrose Tolerance Test. Archives of Internal Medicine. 40 (6), 818–830
- Sweeney, J. S. (1928) A comparison of the effects of general diets and of standardized diets on tolerance for dextrose. Archives of Internal Medicine. 42 (6), 872–876.
- Jacob, S. et al. (1999) Association of Increased Intramyocellular Lipid Content With Insulin Resistance in Lean Nondiabetic Offspring of Type 2 Diabetic Subjects. Diabetes. 48 (21), 1113–1119.
- Bachmann, O. P. et al. (2001) Effects of Intravenous and Dietary Lipid Challenge on Intramyocellular Lipid Content and the Relation With Insulin Sensitivity in Humans. Diabetes. 50 (13), 2579–2584.
- Pimentel, D. (1997) U.S. could feed 800 million people with grain that livestock eat, Cornell ecologist advises animal scientists | Cornell Chronicle [online]. Available from: https://news.cornell.edu/stories/1997/08/us-could-feed-800-million-people-grain-livestock-eat (Accessed 1 March 2018).