Rheumatoid Arthritis and Fibrin
Chronic inflammation is associated with many diseases and conditions. There are many inflammatory markers that can be measured. C-Reactive Protein is one common but non-specific maker. Fibrinogen is another marker of inflammation.
A glossary is shown at the end of the article.
Below is a list of common markers that were used in a 2003 study that examined a number of inflammatory markers associated with heart disease. These included:
- Soluble adhesion molecules (E-selectin, P-selectin, intracellular adhesion molecule-1, vascular cell adhesion molecule-1)
- Cytokines (Interleukin-1, Interleukin-6, Interleukin-8, Interleukin-10 and tumor necrosis factor)
- Fibrinogen
- Serum Amyloid A (SAA)
- high-sensitive C-Reactive Protein (hs-CRP)
- White blood cell (WBC ) count
hs-CRP and fibrinogen are the inflammatory markers with the strongest association of the risk of recurrence of cardiovascular disease. 1
However inflammation is only a moderate indicator of heart disease. Atherosclerotic conditions can occur when hs-CRP is normal (<1 mg/dL). Highest levels of hs-CRP occur with rheumatoid arthritis and systemic lupus erythematosus. 2
Filaggrin is a protein that binds to keratin. Keratin is the main component of the outer layer of skin, hair, nails as well as horns, feathers, claws and hoofs. Antifilaggrin antibodies (AFA) are a strong indicator of rheumatoid arthritis. Two products that are derived from fibrin (deiminated α and β fibrinogen chains) are deposited in the rheumatoid membranes that are a target for the antifilaggrin antibodies. Antibodies are produced by the immune system in response to a foreign invader (called an antigen). In this case, the foreign invaders are the two fibrin-derived products. 3 4 5
This shows that fibrin is implicated in the inflammation resulting in rheumatoid arthritis but does not show the original cause of the inflammation that caused the increase in fibrin and fibrinogen in the first place.
Rheumatoid arthritis is strongly associated with urinary tract infections. This is consistent with the observation that rheumatoid arthritis occurs much more frequently in women.
The majority of urinary tract infections are caused by Escherichia coli (E. coli) bacteria followed by the bacteria Proteus mirabilis.
There is evidence that Proteus bacteria is also involved with rheumatoid arthritis. 6 7
Collagen is the most abundant proteins found in mammals and is the main component of connective tissue. It is found in fibrous tissues such as tendons, ligaments, skin, cartilage and bones as well as other organs. It is cartilage and bones that are affected by rheumatoid arthritis.
An amino acid sequence in a protein in Proteus mirabilis is similar to a sequence found in collagen. Antibodies produced to protect us from the Proteus bacteria are inadvertently “protecting” us from the collagen in our joint tissues which leads to joint disintegration. This process is called “molecular mimicry” or “molecular biomimicry”.
These ideas are not new. A 1995 paper, Decrease in anti-Proteus mirabilis but not anti-Escherichia coli antibody levels in rheumatoid arthritis patients treated with fasting and a one year vegetarian diet, discusses the same issue. 8
Neutrophils are the most common form of white blood cells. They are produced in the bone marrow. They are involved the the immune response to infection and bacteria. Dead neutrophils are the predominant cells in pus. They are short lived with inactivated neutrophils having a half-life of 5 days. 9
Neutrophils are recruited to the site of injury within minutes following trauma. Neutropenia is a condition that causes a low number of neutrophils in the blood.
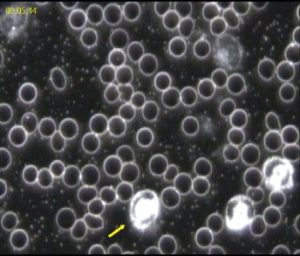
Filgrastim is a synthetic granulocyte colony-stimulating factor (G-CSF) protein that stimulates the growth of neutrophils. Unfortunately, the neutrophils produced in these circumstances can be immature and smaller than the desired size to be effective. Neutrophils are approximately 50-100% larger that red blood cells.
The “hypercoagulable state” refers to a heighten predisposition to form blood clots. “Thrombosis” refers to the formation of blood clots.
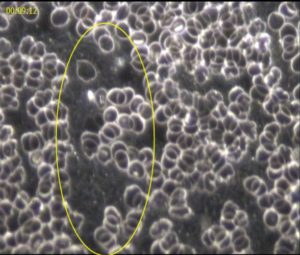
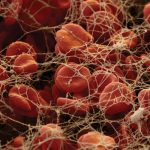
The hypercoagulable state is caused by rapid increase in the production of fibrinogen. Fibrinogen can be seen with a microscope as thin, spider-web like mesh. 11
In a 2013 study, one high-fat meal increased the levels of the 2 inflammatory markers that were measured: Interleukin 6 (IL-6); and tumor necrosis factor (TNF-ɑ) with a maximum increase occurring 8 hours after eating. By this time, most people will have consumed their next high-fat meal. 12
Another study from 2006 showed that when women reduced their intake of fat from 35% to 15%, it resulted in a significant decrease in inflammation markers over a 12 month period. There was a decrease in weight (mean 5.9 kg) and BMI (mean 2.3) and a significant reduction in C-Reactive Protein and LDL Serum Amyloid A. 13
A whole-food, plant-based diet is optimal for reducing inflammation. Chronic inflammation can be indicated by raised fibrinogen and fibrin which can result in debilitating symptoms. Levels of bilirubin higher than the reference range indicate sub-optimal liver function. Chinese herbs can be of benefit to reduce inflammation. 14 15 16
- Fibrin
- A fibrous protein that is involved in the clotting of blood. Fibrin forms a mesh of long insoluble strands that covers the wound. Also referred to as Factor 1a.
- Thrombin
- A protein that involved in the clotting of the blood that causes fibrinogen to join together to fibrin which forms a fibrous mesh to cover a wound.
- Fibrinogen
- A soluble protein that produced by the liver and is found in the blood. Also known as Factor 1.
- Filaggrin
- Filament aggregating protein that binds with keratin which is the major protein component of hair, horns, claws, fingernails and skin.
- Thrombosis
- The formation of a blood clot in a vein or artery. If a blood vessel is injured, platelets (thrombocytes) and fibrin combine to form a blood clot.
- Serum Amyloid A (SAA)
- A group of proteins that are associated with HDL particles that are produced by the liver in response to inflammation.
- C-reactive protein (CRP)
- A protein produced by the liver in response to inflammation.
- Soluble cell adhesion molecules
- A class of proteins that bind to the surface of cells such as platelets in the inflammatory response.
- Cytokines
- Cytokines are small proteins that include interferons, interleukins and tumour necrosis factors. They are involved in immune system signaling that recruit other cells to mount an immune system response. Interleukins (IL) are a group of approximately 50 small proteins that can exert both inflammatory and anti-inflammatory properties. IL-1, IL-6 and tumor-necrosis factor (TNF) are the main inflammatory cytokines.
- Interleukin 6 (IL-6)
- IL-6 is responsible for initiating the acute phase response to an immune system threat. It increases the production of neutrophils in the bone marrow and supports the growth of B-cells in the bone marrow.
- Tumor-necrosis Factor (TFN)
- TNF is involved in the regulation of immune cells. TNF induces fever, programmed cell death (apoptosis) and inflammation. It inhibits tumor growth and viral replication. It responds to infections via IL-1 and IL-6 signalling.
- White Blood Cells (WBC)
- Cells of the immune system that protect the body against foreign invaders (antigens). The main types of cells are neutrophils, eosinophils, basophils, lymphocytes and monocytes. Also called leucocytes.
- Neutrophils
- A white blood cell that is the first to arrive at the site of an infection. Neutrophils help fight infection by ingesting microorganisms and releasing enzymes that kill the microorganisms.
- Antibody
- A protein that is produced in response to a specific foreign body (an antigen). There are 5 classes of antibodies: IgA; IgD; IgE; IgG; IgG. The antigens may be bacteria, viruses, foreign proteins, carbohydrates or other substances that has been recognised as foreign. The antibody is like a jigsaw piece that joins with the matching antigen. The immune system removes the combined antigen-antibody complex (or immune complex) in a number of different ways. At times, the new immune complex can become an antigen (or foreign body).
- Bilirubin
- A product of the breakdown of haemoglobin which occurs when red blood cells are broken down in the liver. It is responsible for the yellow colour of the skin in jaundice. High levels in the blood can indicate liver dysfunction. For several days after birth, bilirubin is much higher than in adults.
Related articles
Rheumatoid Arthritis – an Autoimmune Condition
Rheumatoid Arthritis and Fibrin
Autoimmune diseases and Biomimicry
Our Immune System
Strategies to Assist with Arthritis
Last updated on Tuesday 16 January 2024 at 06:01 by administrators
Footnotes
- Pearson, T. A. (2003) Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice: A Statement for Healthcare Professionals From the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 107 (3), 499–511.
- Roberts, W. C. (2010) It’s the cholesterol, stupid! American Journal of Cardiology. 106 (9), 57–73.
- Citrullination or deimination is the conversion of the amino acid arginine in a protein into the amino acid citrulline.
- Masson-Bessiere, C. et al. (2001) The Major Synovial Targets of the Rheumatoid Arthritis-Specific Antifilaggrin Autoantibodies Are Deiminated Forms of the α– and β-Chains of Fibrin. The Journal of Immunology. 166 (6), 4177–4184.
- van Beers, J. J. et al. (2010) Mapping of citrullinated fibrinogen B-cell epitopes in rheumatoid arthritis by imaging surface plasmon resonance. Arthritis Research & Therapy. 12 6), R219.
- Ebringer, A. (2009) Rheumatoid arthritis is caused by Proteus: The molecular mimicry theory and Karl Popper. Frontiers in Bioscience. E1 (2), 577–586.
- Ebringer, A. & Rashid, T. (2014) Rheumatoid arthritis is caused by a Proteus urinary tract infection. Apmis. 122 (5), 363–368.
- Kjeldsen-Kragh, J. et al. (1995) Decrease in anti-Proteus mirabilis but not anti-Escherichia coli antibody levels in rheumatoid arthritis patients treated with fasting and a one year vegetarian diet. Annals of the rheumatic diseases. 54 (3), 221–224.
- Pillay, J. et al. (2010) In vivo labeling with 2H2O reveals a human neutrophil lifespan of 5.4 days. Blood. 116 (4), 625–627.
- Gutierrez-Delgado, F. & Bensinger, W. (2001) Safety of granulocyte colony-stimulating factor in normal donors. Current opinion in hematology. 8 (3), 155–160.
- Anon (2011) Fibrin Clot. [online]. Available from: https://medicalstate.tumblr.com/post/4535755510/fibrin-clot-fibrinogen-typically-a-soluble.
- Miglio, C. et al. (2013) Antioxidant and inflammatory response following high-fat meal consumption in overweight subjects. European Journal of Nutrition. 52 (3), 1107–1114.
- Kasim-Karakas, S. E. et al. (2006) Responses of inflammatory markers to a low-fat, high-carbohydrate diet: effects of energy intake. The American Journal of Clinical Nutrition. 83 (4), 774–779.
- Chan, E. (1993) Displacement of Bilirubin from Albumin by Berberine. Neonatology. 63 (4), 201–208.
- Wang, B. (2000) Treatment of chronic liver diseases with traditional Chinese medicine. Journal of Gastroenterology and Hepatology. 15E67–E70.
- Huang, W. et al. (2004) A traditional herbal medicine enhances bilirubin clearance by activating the nuclear receptor CAR. Journal of Clinical Investigation. 113 (1), 137–143.




.
Hello Gloria
I advocate a whole-food, plant-based diet. Supplements may be useful and essential in some circumstances but I fail to see the benefits in taking Metamucil which contains Psyllium fibre.
Psyllium can cause bloating and cramps. It is important to ensure that sufficient water is consumed. Some people can have an allergy to Psyllium which can be severe.
Instead of taking supplements, people are much better off obtaining their fibre from whole grains, beans, fruit and vegetables.
There are a number of clinical trials comparing Psyllium with prunes for the treatment of constipation. One such study concluded “Dried plums are safe, palatable and more effective than psyllium for the treatment of mild to moderate constipation, and should be considered as a first line therapy”. [1]
[1] Attaluri, A. et al. (2011) Randomised clinical trial: dried plums (prunes) vs. psyllium for constipation: Randomised clinical trial: dried plums in constipation. Alimentary Pharmacology & Therapeutics. 33 (7), 822–828.